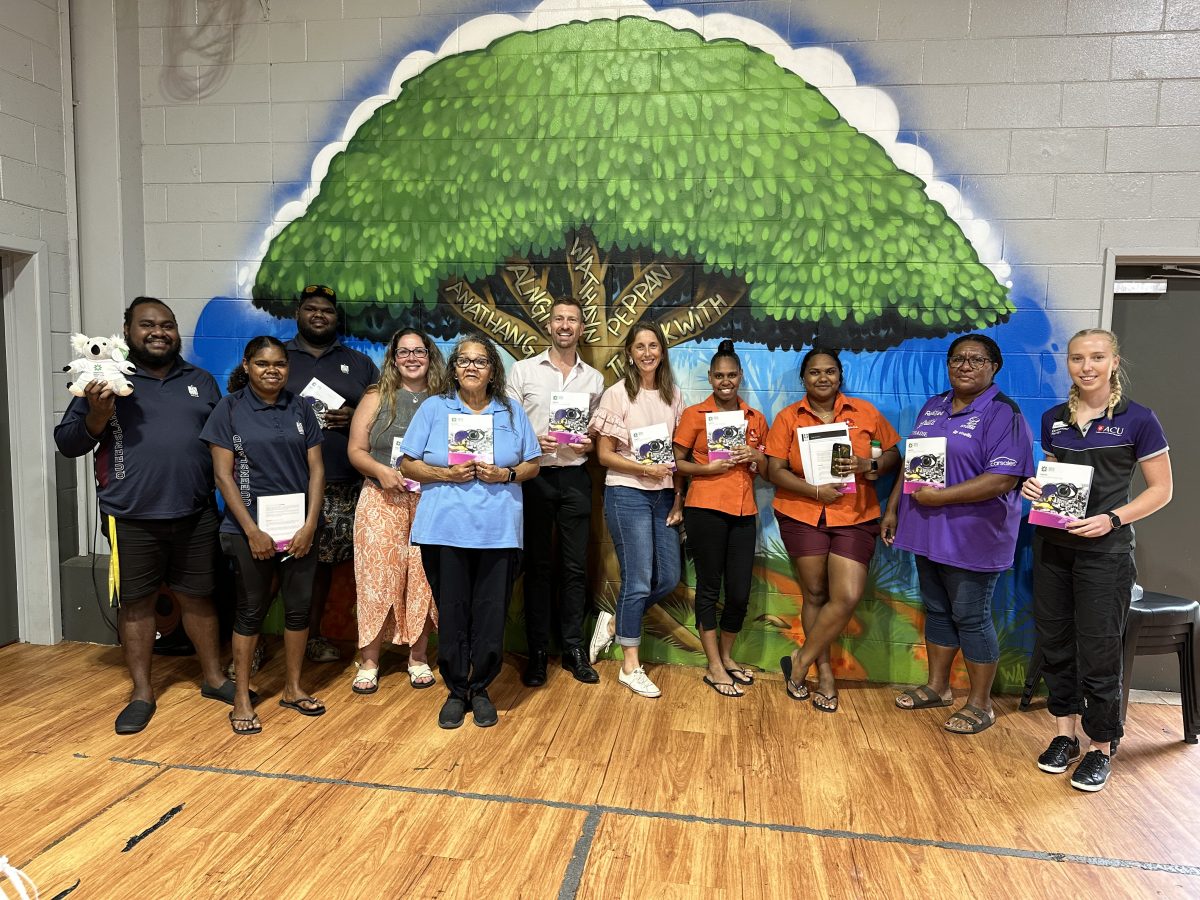
Service providers from Napranum and surrounding western Cape York communities attended the recent mental health first aid training course. Photo: Supplied.
Most people are familiar with the concept of physical first aid, but in a remote community where it can be weeks before a mental health professional is available, mental health first aid is just as important.
Mental Health First Aid Australia shared a practical, skills-based action plan to support youth experiencing a mental health crisis when it hosted a 14-hour course at PCYC Napranum on 8-9 May for those wanting to learn about issues prevalent to youth in the 12-18 age bracket.
Course participant Kathryn Sealey, who works at Weipa Community Care, said access to mental health support could be challenging in remote areas.
“I think mental health, especially in rural areas, is huge,” she said.
“There are organisations in the area, but a lot of people do FIFO (fly-in, fly-out), so instead of just being able to have an appointment the next day or in a few days, it can be a couple of weeks.”
Ms Sealey said she learned a lot and was looking forward to passing on the knowledge to her colleagues.
“One thing that was shocking to me was the statistics of young people and their mental health conditions,” she said.
“I guess they’re suffering and not necessarily knowing how to get help, so it was really good to learn the early signs so that we’re able to address it.”
Workshop facilitator Teresa Gibson from the Royal Flying Doctor Service said participants were taught the ALGEE action plan.
The plan consists of assessing for risk, listening non-judgementally, giving reassurance, encouraging professional help, and encouraging other support strategies.
“Access is not always there in community, so it’s about keeping the young person safe until professional help arrives,” Ms Gibson said.
Co-facilitator from Queensland Health, Nic Madgwick, said two in five young people had poor mental health.
“We cover topics such as depression, anxiety, eating disorders, psychosis, and substance abuse disorders with a focus on how to manage any crisis,” he said.
“Those crises include suicide, non-suicidal self-injury, panic attacks, traumas, and also any medical emergency.”
Over the two days, Mr Madgwick said he saw great progress in the participants’ confidence in providing mental health support.
“Some of the reactions that we’ve received from the participants is an increased awareness and understanding around what mental health looks like, where before, they might not have picked up on early warning signs of what depression or anxiety looks like,” he said.
“They’re saying that the information provided here is very useful and they’ll be able to take it back and use it within their environments where they’re employed.”

Course facilitator Teresa Gibson, participant Kathryn Sealey and facilitator Nic Madgwick reflect on key learnings at the conclusion of the two-day youth mental health first aid training at PCYC Napranum. Photo: Supplied.








